By Avigayil Kadesh
On August 8, the World Health Organization declared the West African Ebola epidemic, which has killed about 1,000 people, an international public-health emergency. It called upon member states and private donors to expend greater resources toward finding a cure for the worst Ebola outbreak in history. Currently there is no vaccine or cure.
Significant gains in this field are happening in Israel, where Dr. Leslie Lobel and Dr. Victoria Yavelsky have been working for years to track down all survivors of the Ebola and Marburg viruses in Uganda and take blood samples from them. Both of these Equatorial viruses cause hemorrhagic fever and kill close to 90 percent of victims.
The two scientists study the unusually strong immune response of the survivors and then work to isolate monoclonal antibodies that neutralize the virus in their lab at Ben-Gurion University of the Negev’s Center for Emerging Diseases, Tropical Diseases and AIDS.
Yavelsky and Lobel’s monoclonal antibody-based therapeutic approach was proven as a successful potential treatment by their colleagues in the US military, and at several other laboratories.
With funding from the US National Institutes of Health and other resources, their lab is now getting ready to test its human monoclonal antibodies in mice and non-human primates abroad.
“We have a five-year plan and I believe we could have proof of concept with human monoclonal antibodies in monkeys in three to five years,” Lobel predicts. “If we can prove it in two animal models we can eventually use it in humans.”
Prevention and cure
Lobel, a 2002 American immigrant educated at Columbia University, notes that the work being done at Ben-Gurion University is essential since there are few studies on survivors of Ebola. When someone contracts Ebola, it usually takes eight to 12 days for symptoms of hemorrhagic disease to show up. The antibody therapy could provide not only a cure but even prevent the hemorrhagic disease from occurring in the first place.
“We’re quite advanced in terms of studying the immune response in survivors in Central Africa to develop a prophylactic and therapeutic,” says Lobel, who travels to Uganda for his work about five times a year.
“We have set up a base laboratory in Entebbe, with our Ugandan colleagues, so that we can process human blood samples in under 12 hours from the time of collection, which is required for our work. After the samples are tested and deemed to be non-infectious, we ship them to Israel and our team here develops antibodies from the samples.”
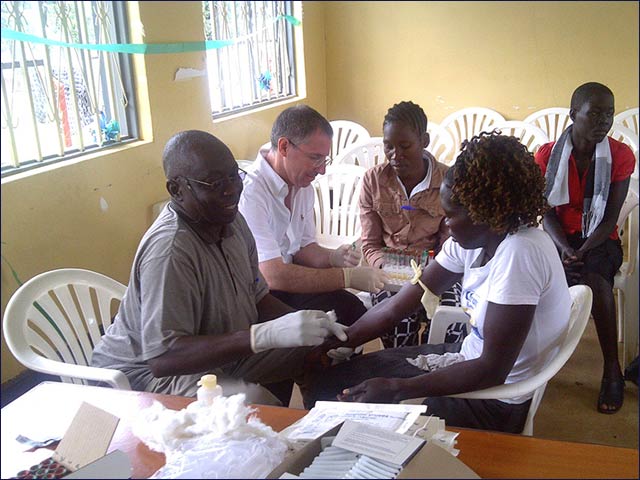
Dr. Lobel and colleagues collect samples from Ebola survivors in Uganda He and Yavelsky hope to develop a “passive” vaccine that would provide immediate protection against the virus. An “active” vaccine already formulated by the US military, and successfully tested in monkeys, takes about 30 days to be effective.
The current outbreak was first noticed last February in Guinea, a country that is normally outside the usual ecosystem for Ebola, according to Lobel. At the end of March, the US Centers for Disease Control sent a team to assist Guinea Ministry of Health and World Health Organization in formulating an international response to the outbreak that is now affecting other African countries including Sierra Leone, Liberia and Nigeria.
Meanwhile, several other experimental vaccines and therapeutic approaches to Ebola and Marburg – mostly in the United States and Canada – are in various stages of study. In Israel, Vecoy Nanomedicines is developing a biomedical technology platform that tricks a virus into “committing suicide,” which could neutralize viral threats like Ebola, hepatitis and HIV. However, Vecoy’s Dr. Eitan Eliram says that Vecoy has not yet found sufficient funding to go forward with its research and development.